General Content
Rochester Regional Health investigates and tracks several metrics related to mortality. After each patient death, a quality review is performed examining the severity of illness and to look for potential process opportunities Rates that are tracked include overall inpatient mortality and disease specific survival rates. Hospitals evaluate their inpatient mortality rates by using an index value of observed mortality to expected mortality.
Measures related to mortality are important to track because they identify opportunities for improvement in care and care variation. Some illnesses have much lower expected mortalities rates than others, so if a patient expires from one of those unlikely causes, the Rochester Regional Health team wants to learn why to help improve future patient care.
During the hospital stay, inpatient falls occur when any patient has an unplanned downward movement to the floor. They are mostly avoidable events, and when they happen, there is potential for the patient to experience harm (fracture after the fall). The risk of falls increases with age, unfamiliar settings, medications that might cause dizziness or confusion, or illness and treatments that might make some patients weak or unsteady. Falls with serious injury increase the risk of avoidable complications and often require longer hospital stays.
Measures related to patient falls, such as Patient Safety Indicator 08 (PSI 8), and Hospital Fall with Hip Fracture, are important to track to understand opportunities for improvement and prevent future harm. Efforts to prevent falls include assessing if a patient is at risk for a fall and taking action to make every effort to stop the fall from happening.
PSI 8 is a publicly reported measure and is part of a larger measure set called PSI 90 which monitors healthcare complications for all hospitals across the United States. The data is reported as rates (number of falls divided by total patient days then multiplied by 1,000) to compare hospitals’ performance and can be found on the Leapfrog hospital grade site.
PSI 8 captures hospital falls with hip fractures, but does not include any patients that are admitted with the following conditions: seizure disorder, syncope, stroke, occlusion of arteries, coma, cardiac arrest, poisoning, trauma, delirium or other psychoses, anoxic brain injury, diagnoses associated with fragile bone, patients admitted with a hip fracture, and obstetric cases. Please note Leapfrog data for this measure time period is 2 years behind our current data or performance. PSI 8 is labeled as “falls causing broken hips” and includes discharges between 07/01/2019 - 12/31/2019 and 07/01/2020 - 06/30/2021.
click on any hospital below to find the Leapfrog data.
Below, we show recent data on falls with hip fracture for all RRH hospitals in 2 graphs. The first graph shows the fall rate (number of falls divided by total patient days then multiplied by 1,000 as reported in Leapfrog) comparing performance from 2022 to 2023 Quarter 1.
Current Fall Rates with Hip Fracture January 1, 2022-March 31, 2023
(Number of falls divided by total patient days multiplied by 1000)
| Rochester Regional Health Hospitals | 2022 | Q1 2023 |
| Clifton Springs Hospital | 0.00 | 0.00 |
| Canton Potsdam Hospital | 0.15 | 0.00 |
| Massena Hospital | 0.18 | 0.00 |
| Newark Wayne Community Hospital | 0.00 | 0.00 |
| Rochester General Hospital | 0.19 | 0.19 |
| United Memorial Medical Center | 0.30 | 0.00 |
| Unity Hospital | 0.49 | 0.00 |
| Gouverneur Hospital | 0.00 | 0.00 |
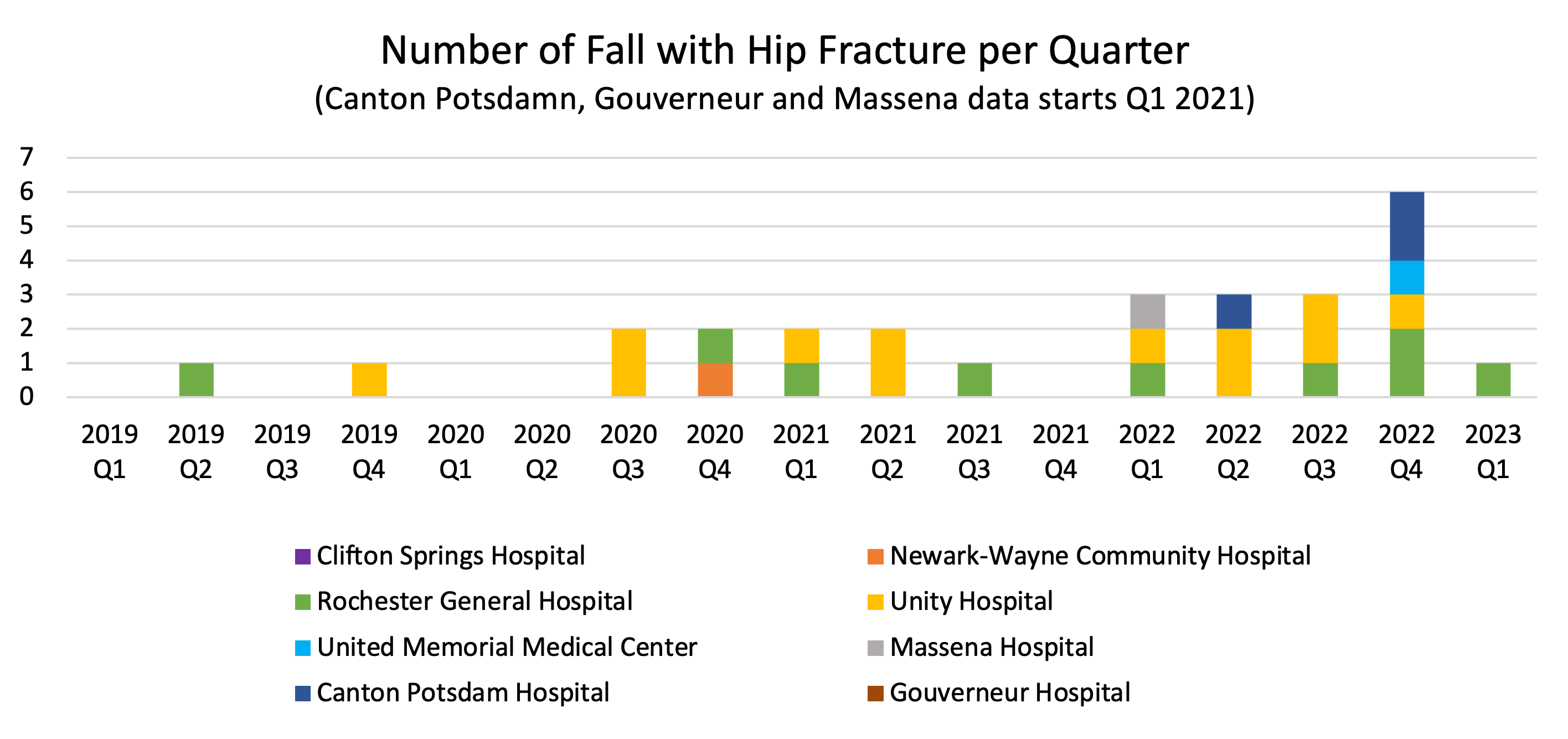
The second graph shows the actual number of falls with hip fractures that occurred at all Rochester Regional Health (RRH) hospitals. Note, the table below includes all falls (including all previously excluded PSI 8 as noted above).
All Rochester Regional Health Hospitals are dedicated to preventing patient falls and associated injuries.
To identify patients at higher risk of falls, the clinical team proactively completes a fall risk screen on all patients. In quarter 1 of 2023, RRH implemented a fall predictive tool that uses advanced technology to continuously scan the patient’s medical record to predict the patient’s fall risk. This was considered to provide a more accurate and timely indication of risk than previous assessments, which were only done at shift changes and could be time-consuming and difficult to complete. If a patient is identified as a high fall risk, an action plan and interventions are activated to make every effort to prevent the fall from happening.
Here is a list of best practices implemented when a patient is identified as a fall risk:
Wherever care is provided by Rochester Regional Health System, quality and patient safety are top priorities. This information is being shared to educate our community about patient falls and all efforts to prevent falls across Rochester Regional Health.
Healthcare-associated infections (HAIs) are infections that a patient develops while in the hospital, related to the care received. Devices such as central lines and foley catheters, surgical procedures and antibiotic use pose a risk of infection to the patient, so the use of them must balance the need for the device or procedure with the associated risk. HAIs are events that have the potential to cause significant patient harm. Catheter Associated Urinary Tract Infections (CAUTI), Central Line Associated Blood Stream Infections (CLABSI), Clostridium difficile (C.diff) infection, Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, and Surgical Site Infections (SSIs) are important healthcare-associated infections that are routinely assessed and reported to state and federal agencies as required.
HAIs are avoidable harms that occur in the healthcare setting. Patients who acquire HAIs have increased length of stay compared to those without HAIs and have poorer outcomes. Preventing HAIs is the focus of the Infection Prevention Program.
Hand hygiene is cleansing hands using either soap and water or alcohol hand rub. Hand hygiene is the single most effective way to prevent the spread of infection. Hand hygiene is performed during these five moments* of patient care:
![]()
Hand Hygiene is the most important action against spreading infection from person to person.
* World Health Organization Five Moment of Hand Hygiene
Readmissions occur when a patient needs to come back to the hospital for an inpatient stay. Generally, hospitals track 30-day readmission rates for the overall hospital as well as disease specific conditions, but other readmission time frames can also be looked at and are important to be looked at.
Tracking readmission rates provides information about the initial visit care and what our healthcare providers may need to do to keep patients healthy once they leave the hospital.
Patient safety indicators are specific quality indicators that look at occurrences of harm to patients. Collectively the measures are rolled up into a composite score known as PSI-90. These indicators include measures such as accidental punctures and lacerations to post-operative hip fractures. The system also reviews other hospital acquired conditions (HACs) that are even broader than the PSI-90 measures, but are still conditions developed while receiving care in the hospital.
Any type of harm that is incurred while in the hospital is potentially avoidable. Given proper attention and education on these measures, hospitals strive to make these events never occur.
Clinical process of care or quality measures are specific measures set forth by regulatory bodies (such as the Center for Medicare/Medicaid Services or CMS) that look at how frequently certain events occur. For example, elective deliveries prior to 39 weeks gestation without medical necessity are generally discouraged. Measuring how frequently and why this event may occur helps to promote better care for our next patient.
Measuring how frequently and why this event may occur helps to promote better care for our next patient.
Patient satisfaction measures are indicators that tell hospitals how patients perceive the care they received in the hospital.
Patient satisfaction measure help identify areas of strength and opportunity for hospitals to help provide better care to patients. It also helps tell hospitals and providers if the message they are trying to share with patients is being received appropriately. Care has the best outcome if patients feel supported in their care.